Brief overview: What is social freezing and how does it work?
Social freezing is the removal and freezing (cryopreservation) of a woman’s eggs at a young age to preserve fertility for a longer period of time. Frozen eggs can later be used in artificial insemination without any specific medical reasons. As a rule of thumb, due to the decreasing number and quality of available eggs with increasing age, social freezing should be performed up to the age of 35. The reason for performing social freezing is the sharp decline in fertility in women from about 35 years of age.
The procedure of social freezing is similar to that of artificial insemination (IVF / ICSI method) without fertilization being performed with the retrieved fresh eggs:
First, a woman’s egg maturation is stimulated with hormone treatment. Ideally, up to 30 follicles of eggs will mature at a time, however, fewer eggs may mature and additional cycles may be needed to reach the target total number of frozen eggs.
Then ovulation is induced by medication and a few days later the eggs are retrieved. In this procedure, the matured oocytes are removed from the follicles through the vagina by puncture.
Finally, the retrieved unfertilized eggs are frozen and stored. Reproductive physicians recommend storing about 20-30 unfertilized eggs to increase the likelihood of success in a future childbearing attempt.
At a later stage, the cryopreserved eggs can then be thawed and fertilized in an artificial insemination (IVF / ICSI method) and transferred to the woman’s uterus to initiate pregnancy.
When does social freezing make sense?
This is a question that women should always answer for themselves – however, a few food for thought from a medical, social and legal point of view should be given here.
From a medical point of view, the rule is that social freezing should be carried out up to the age of 35 and that the earlier social freezing is carried out, the more promising it generally is.
When social and legal considerations are taken into account, the ideal age to perform social freezing is between 31 and 35, as women in their late 20s still have time to consider the option of social freezing without risking significant loss of fertility (this usually begins in the mid-30s). In addition, in Switzerland and other countries there are legal restrictions on how long the retrieved eggs may be stored, in Switzerland this is 10 years. Therefore, it rarely makes sense to freeze eggs well before the age of 35, unless there is a risk of premature ovarian failure.
Another reason for egg freezing is cancer, as women often become infertile due to chemotherapy treatment. In this case, however, physicians do not speak of social freezing, but of fertility preservation for medical reasons. In such cases, health insurance often covers the cost of treatment.
Who uses social freezing?

Young women who currently do not want to get pregnant (e.g. due to a lack of a partner) or want to postpone the decision (e.g. for career reasons) can consider social freezing.
It is important that women are aware of the additional costs associated with social freezing. This is not only about the immediate costs of social freezing at the time of implementation, but also about the additional costs that arise when the frozen eggs are used in the context of artificial insemination.
How does egg freezing work?
In some cases, several cycles of social freezing treatment are needed to ensure a sufficient number of frozen eggs – experts recommend freezing up to 20-30 eggs.
Hormonal stimulation of the ovaries

Typically, for social freezing, a woman must undergo hormone stimulation to mature a larger number of eggs that can be frozen.
First, hormone preparations prevent the woman’s natural ovulation.
Depending on the protocol, egg stimulation begins up to 14 days later. The aim of stimulation is that several follicles mature at the same time.
Depending on the individual situation of the woman, different hormone preparations are used for hormone treatment, which are injected or also taken as tablets. The hormone FSH (follicle stimulating hormone) is often injected, which can either be injected by the woman herself or by another person.
Hormonal stimulation of the ovaries should be closely monitored by a physician, as overstimulation of the ovaries may occur in rare cases.
Triggering ovulation and egg retrieval
Approximately one week after starting hormone treatment, a doctor will perform an ultrasound examination to check the size and maturity of the developing eggs. In addition, certain hormone levels in the blood are measured. If the eggs have matured successfully, the hormone treatment is now stopped. Ovulation is then induced by injecting certain hormones or drugs (e.g. human chorionic gonadotropin or GnRH agonists) approximately 9-11 days after the start of hormone treatment.
36 hours after ovulation is induced, the so-called follicular puncture is performed. In this procedure, the doctor removes mature oocytes from the follicles using a fine needle. Usually this procedure is performed under light anesthesia through the vagina.
Freezing and storage
The retrieved oocytes are stored at -196° Celsius in a so-called cryobank. This process is also called vitrification. In the cryobank, the eggs are stored in liquid nitrogen until they are either used for artificial insemination or destroyed.
Experts believe that frozen eggs could be stored in this way almost indefinitely, although there are some legal restrictions (e.g. maximum storage period of 10 years in Switzerland) or biological restrictions on the woman – after a certain age, even the transfer of thawed eggs only leads to the desired result with a low probability. However, a woman can still get pregnant with the frozen eggs after menopause, although the risks for mother and child increase with the woman’s age.
Later: thawing, fertilization and embryo transfer
If the woman wants to use the frozen eggs, e.g. when she has found the right partner or as part of a sperm donation, they are first thawed.
Fertilization of the eggs is then usually performed by in vitro fertilization (IVF) or intracytoplasmic sperm injection (ICSI). For this purpose, the unfertilized eggs are mixed with sperm cells from the partner or a sperm donor in a nutrient fluid and placed in an incubator – here fertilization is to occur.
The eggs are then removed from the incubator and, if fertilization is successful, 1-2 embryos are selected to be transferred to the woman’s uterus, where they ideally implant.
Surplus fertilized eggs can be stored with cryopreservation for possible further attempt or further pregnancies.
What are the opportunities and risks of social freezing?
Probability of success of a live birth

Two factors are central to whether social freezing is successful in terms of live birth: the number of eggs retrieved and frozen, and the age of the woman at the time of transfer of the thawed and fertilized egg.
Scientists have developed a model to help women decide how many eggs to freeze. Based on this model, the following graph provides an overview of how the probability of a live birth changes depending on the number of frozen eggs and the age of the woman at the time of egg transfer.
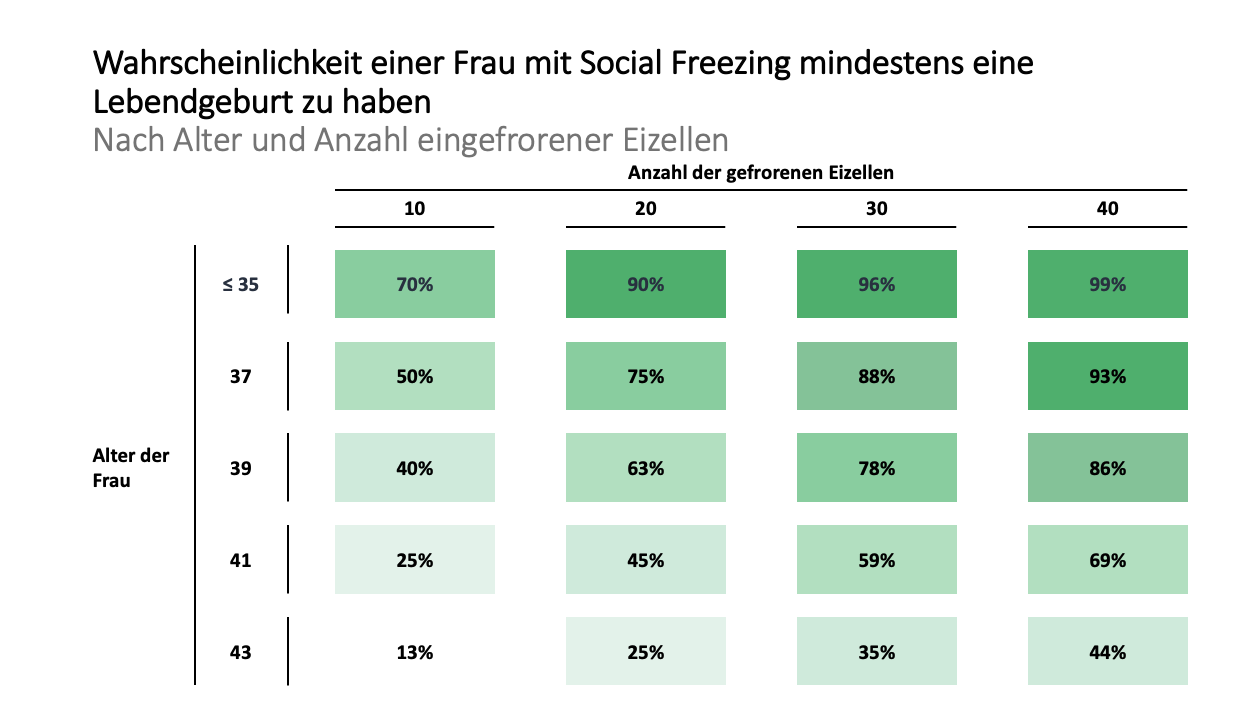
Source: Goldman et al. (2017)
It is striking that the age of the woman is also a decisive factor for the success of social freezing and that the success of the treatment is by no means guaranteed. For example, with 20 frozen eggs, the probability of at least one live birth decreases with age. This is 90% when the woman is 34 years old and 75% when she is 37 years old. at age 41 at 45% and at age 43 only 25%.
Risks for the health of the child
Scientists believe that the use of cryopreserved eggs in itself does not pose a risk to the health of the child compared to the use of fresh eggs.
However, data on this is incomplete and relatively few long-term studies are available, as the technique of cryopreservation is still relatively new. Therefore, it cannot be said with absolute certainty whether children conceived after social freezing have a higher risk of malformations.
Side effects of hormone treatment
Side effects may occur in the course of hormonal stimulation. Typical symptoms are hot flushes, dizziness and visual disturbances. In the worst case, ovarian hyperstimulation syndrome may develop.
Ovarian hyperstimulation syndrome
Hormonal stimulation of the maturation of multiple eggs can cause ovarian hyperstimulation syndrome, which causes the ovaries to swell and hurt. In severe cases, this can become life-threatening.
In the past, ovarian hyperstimulation syndrome occurred in up to 10% of women undergoing hormone stimulation; today, this number is less than 5%; serious cases of ovarian hyperstimulation syndrome occur in less than 1% of women undergoing hormone therapy.
Symptoms of ovarian hyperstimulation syndrome include a distended abdomen, pain, nausea, and shortness of breath.
High-risk pregnancies from 35
Pregnancies in which the expectant mothers are 35 or older are considered high-risk pregnancies in Switzerland, Germany and Austria. Especially pregnant women in the “older age” over 40 may experience problems during pregnancy for mother and child. The older the expectant mother, the higher the mother’s risk of gestational toxicity (gestosis), gestational diabetes, cardiovascular disease, and the risk of malformations and premature or stillbirth of the child.
However, this risk does not simply depend on the mother’s age; doctors look in particular at whether there has already been a previous (complication-free) pregnancy and what the expectant mother’s general state of fitness and health is like. With a previous pregnancy and a good level of fitness and health, a 40-year-old’s pregnancy is officially considered a high-risk pregnancy, but in reality it doesn’t have to be.
Nevertheless, expectant mothers over 35 are advised to seek closer medical care and support during pregnancy than would be the case for a younger woman.
How much does social freezing cost?
Costs in Switzerland and Europe
Switzerland
In Switzerland, a social freezing cycle costs approximately CHF 4,000 to CHF 5,000. Added to this are costs for
- Hormones to stimulate the oocytes – these cost CHF 1,000 to CHF 2,000 per cycle, depending on the hormone and the amount required
- the freezing and storage of the oocytes of about CHF 700 in the first year and about CHF 400 per year in the following years
To obtain 20-30 oocytes, 2-3 cycles may well be necessary, thus increasing the costs to CHF 12,000 and more.
These costs must be borne by patients themselves; Swiss health insurers do not cover them. An exception here is for the freezing of eggs for medical reasons (especially cancer), in these cases the costs are covered by basic insurance in Switzerland since July 1, 2019 for 5 years.
Germany and Austria
In Germany, the treatment costs for social freezing are around EUR 3,000 to EUR 4,000, plus costs for the hormones to stimulate egg production of between EUR 700 and EUR 1,600, as well as storage costs of EUR ~600 in the first year and EUR ~300 in subsequent years. Furthermore, there is no restriction in Germany regarding the storage period of frozen oocytes.
In Austria, social freezing is not permitted; the freezing of eggs is only allowed for medical reasons, e.g. for fertility preservation in the course of cancer.
Other European Countries
The following table provides an overview of the expected costs for social freezing for Switzerland, Germany and Austria as well as the currently most popular destination countries for medical tourism in the field of fertility.
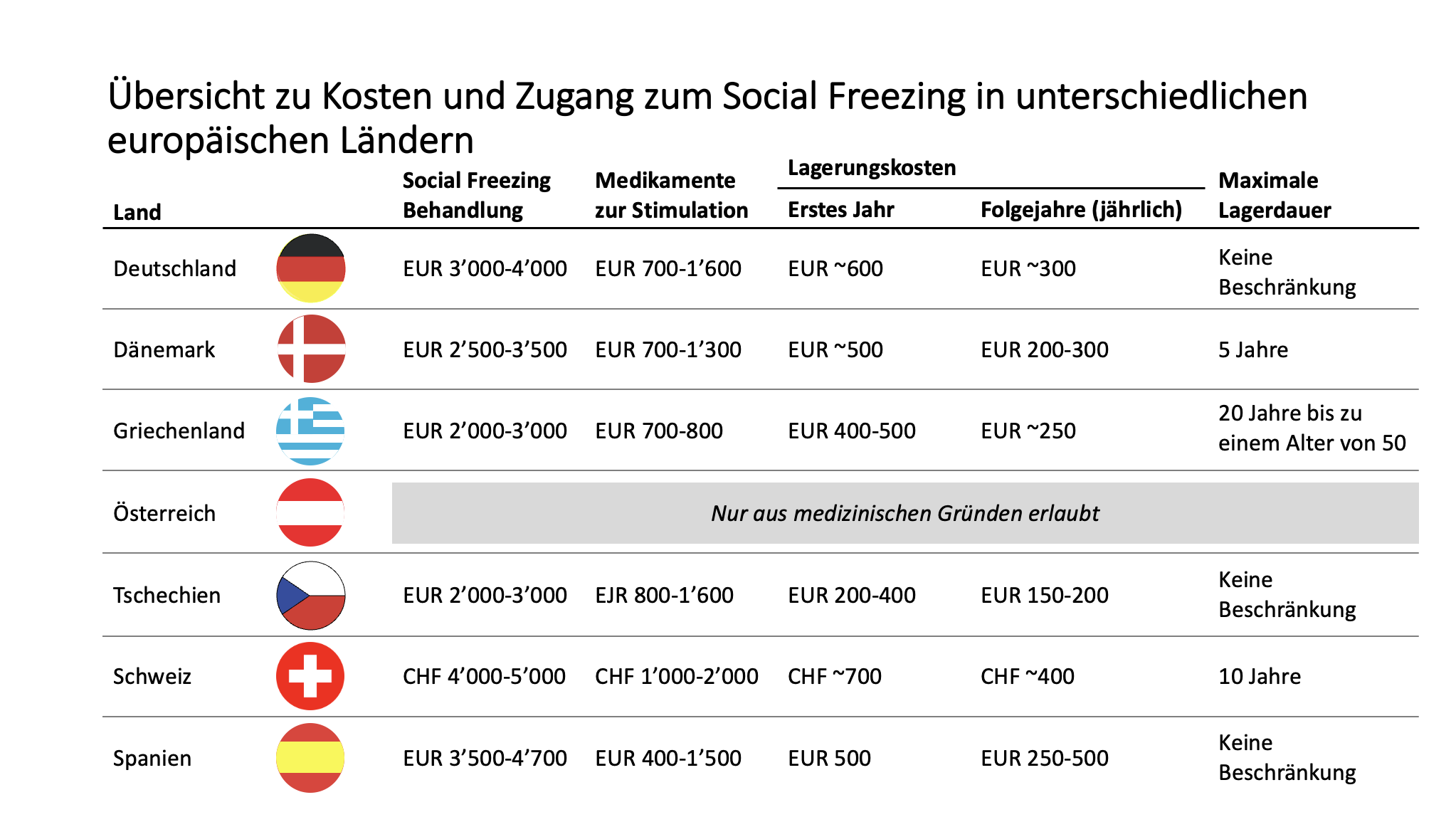
Source: fertilityroad.com, various price lists from local fertility clinics.
Here are a few key observations from the comparison:
- The Czech Republic and Greece are the most favorable countries for performing social freezing, although the costs in the Czech Republic can be even a tad lower than in Greece
- Denmark can also be a relatively inexpensive choice for performing social freezing, but here the maximum storage period is limited to 5 years, which may be too short a time horizon in many cases
- The implementation of a social freezing cycle in Spain can be relatively expensive – this is often more expensive than in Germany and sometimes comes close to the treatment costs in Switzerland
Additional costs for the use of oocytes
Finally, it should be noted that the costs of social freezing do not end with the annual storage costs. For the use of the eggs, patients still have to reckon with the cost of at least one so-called cryocycle. In Switzerland, these total about CHF 1,000-2,500, while in Germany and Austria they are somewhat lower at EUR 800-1,000 and EUR ~1,150, respectively.
Depending on the regulations of the country where the oocytes were frozen and regulations in the home country/a third country, frozen oocytes may also be sent to the home country or a third country for cryocycling, if necessary. However, this is associated with additional costs.
Last update: November 29, 2022
Interested in social freezing, but the cost and hassle scare you off?
Greece is among the European countries with the cheapest fertility treatments. At Kalimedica, we connect you with fertility experts and support you on your social freezing journey



