Brief overview: What is IVF and how does it work?
In vitro fertilization is often colloquially referred to as artificial insemination, although the term actually describes a specific type of artificial insemination in which fertilization does not take place in the woman’s body but in the laboratory.
In vitro fertilization usually takes several weeks. To obtain enough eggs for fertilization, the woman’s egg production is stimulated with hormones at the beginning of the treatment.
After hormone treatment, eggs are removed from the woman’s ovary and mixed in the test tube (= in vitro) with the partner’s sperm (or a sperm donor).
If fertilization is successful, the fertilized eggs (= zygotes) then mature into embryos in an incubator.
Normally, up to 2 embryos are transferred into the woman’s uterus on the 2nd day after fertilization (4-cell stage) or on the 5th day after fertilization (blastocyst stage). Surplus fertilized eggs or embryos can be frozen in liquid nitrogen for later use (cryopreservation).
When should patients consider IVF?
IVF is used in different cases – depending on the cause of the unfulfilled desire for a child:
Cause of unfulfilled desire to have children in women: IVF is used in women with tubal occlusion, endometriosis or antibodies to the partner’s sperm.
Cause of unfulfilled desire to have a child in a man: if the quality of the man’s sperm is so poor that previous intrauterine insemination (IUI) has been unsuccessful, IVF is usually considered as the next stage of treatment.
How does IVF work?

Hormonal stimulation of the ovaries
First, hormone preparations prevent the woman’s natural ovulation.
Depending on the protocol, egg stimulation begins up to 14 days later. The goal of stimulation is to have multiple follicles mature at the same time in order to obtain more eggs for successful artificial insemination.
Depending on the individual situation of the woman, different hormone preparations are used for hormone treatment, which are injected or also taken as tablets. Often the hormone FSH (follicle stimulating hormone) is injected, which the woman can inject herself or can be injected by another person.
Hormonal stimulation of the ovaries should be closely monitored by a physician, as overstimulation of the ovaries may occur in rare cases.
In some cases, hormonal stimulation of the ovaries is not used and the woman’s natural menstrual cycle is used to retrieve the eggs (so-called natural cycle IVF).
Triggering ovulation and egg collection
Approximately one week after starting hormone treatment, a doctor will perform an ultrasound examination to check the size and maturity of the developing eggs. In addition, certain hormone levels in the blood are measured. If the eggs have matured successfully, the hormone treatment is now stopped. Injection of certain hormones or drugs (e.g. human chorionic gonadotropin or GnRH agonists) will then induce ovulation approximately 9-11 days after the start of hormone treatment.
36 hours after ovulation is induced, the so-called follicular puncture is performed. In this procedure, the doctor removes oocytes from the matured follicles with the help of a fine needle. Usually this procedure is performed under light anesthesia through the vagina.
In rarer cases and depending on the individual situation of the woman, the eggs are retrieved by laparoscopy – a surgical procedure through the abdominal wall that is usually performed under general anesthesia.
Fertilization of the oocytes in the laboratory and cultivation
Now the fertilization of the eggs takes place in the laboratory. On the day of egg collection, the eggs are mixed with sperm from the partner (or a donor) in the laboratory, which results in fertilization of the eggs. This requires fresh or frozen sperm from the partner or a donor.
If a male fertility disorder is present, fertilizable sperm can also be obtained via testicular biopsy in certain cases, frozen, and then thawed in a timely manner.
The semen used is often still processed in the laboratory to increase its fertilizing ability and prevent allergic reactions in the woman.
Then eggs and sperm are mixed in a nutrient fluid and placed in an incubator – this is where fertilization is supposed to occur, which is where the treatment gets its name (in vitro fertilization = fertilization in a jar).
After removal of the mixture from the incubator, individual oocytes are examined under the microscope. In this process, experts can tell whether fertilization has been successful by looking at two so-called “pronuclei” that have emerged from the egg cell and sperm cell. Now the eggs are selected that will later be transferred into the uterus. Other fertilized eggs are either destroyed or, if necessary, frozen for later use in a so-called “cryocycle”.
Transfer of 1-2 embryos
One or more successfully fertilized eggs are once again placed in the incubator, where they are allowed to develop for a few days. Between days 2 and 6 after fertilization, 1-2 of the fertilized embryos are then transferred into the woman’s uterus. This is done without anesthesia using a thin and flexible tube (catheter) through the woman’s vagina and is usually little or not painful.
Surplus fertilized eggs can be stored with cryopreservation for possible further attempt or further pregnancies.
Additional treatment: Hatching aid (Assisted Hatching)
In some cases, for example, when several unsuccessful embryo transfers have already been performed or when cryopreserved eggs are used, doctors can try to improve the implantation of the transferred embryos with a so-called hatching aid.
Usually, an embryo must implant in the uterine lining on about the fifth day after fertilization. For this, the outer shell surrounding the embryo must be thin enough for the embryo to hatch out of it. To increase the probability of success here, the outer shell of the embryo is thinned out by laser during hatching.
However, there are no clear results on the improvement of the probability of getting pregnant with this method.

Control examinations
About 2 weeks after embryo transfer, a test of the pregnancy hormone human chorionic gonadotropin (HCG) in the woman’s blood can be used to test whether pregnancy has begun. Usually, several tests are performed to ensure a reliable result.
As with any pregnancy, an embryo or embryos can be detected by ultrasound about a month after the beginning of the pregnancy.
What are the chances and risks of IVF?
IVF treatment is a relatively safe and promising method of artificial insemination. In Europe, more than 900,000 IVF cycles are performed annually and approximately 200,000 children are born with the help of IVF treatment.
Probability of success
The probability of success in an IVF cycle to give birth to a healthy child is 25-30%. However, as with all methods of artificial insemination, it depends on various factors, such as age, number of previous unsuccessful treatments, ovarian reserve, receptivity of the endometrium, etc.
In particular, it should be noted that, as with natural fertilization, the probability of success with IVF treatment decreases more and more with the age of the woman – the following graph illustrates this effect based on data from Germany:
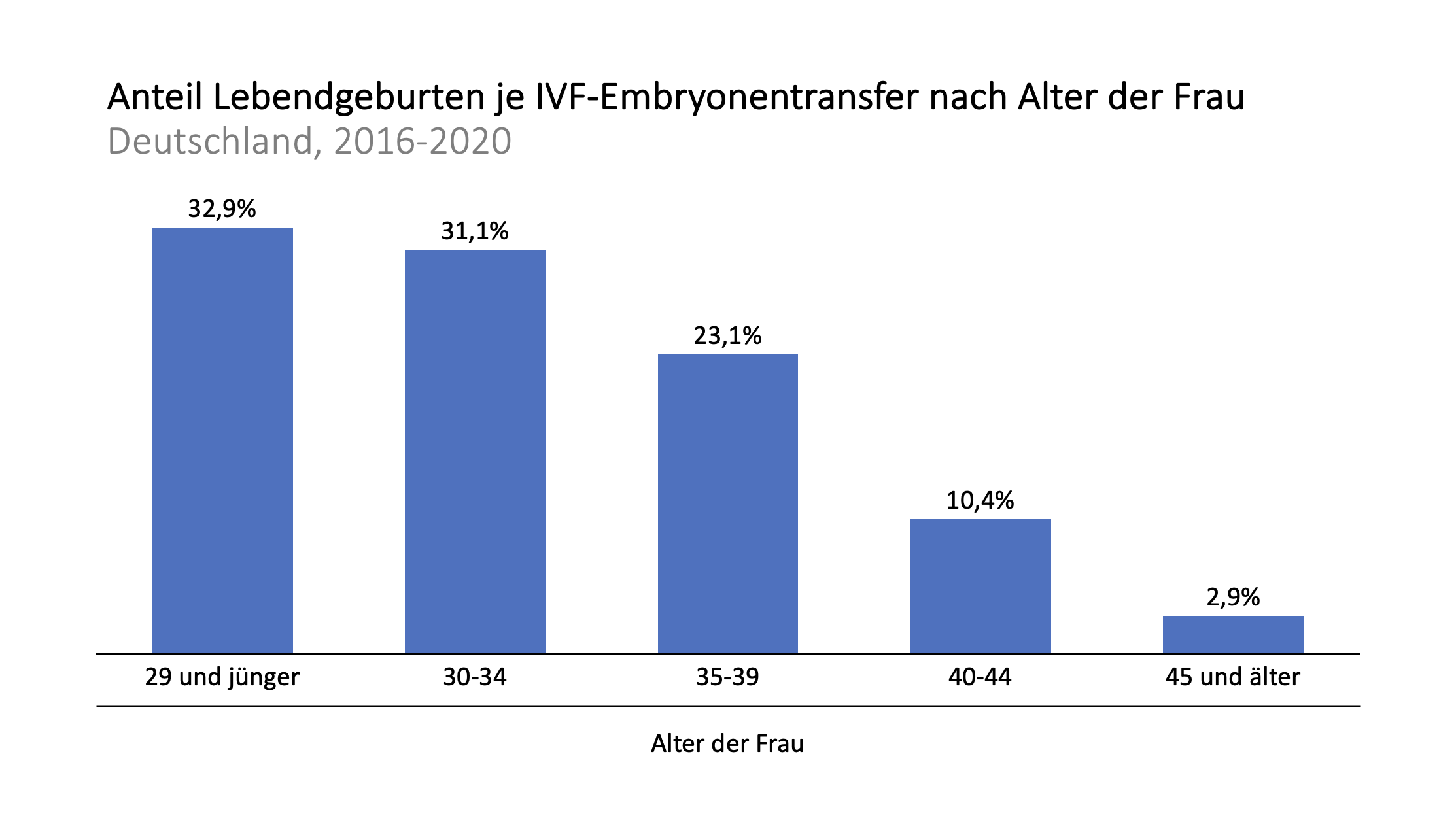
Source: German IVF Register Yearbook 2021
Multiple births
By transferring two embryos instead of one during embryo transfer, the probability of success of an IVF cycle can be increased, as there is a higher chance that one of the embryos will successfully manage the transfer and pregnancy. Especially in older women, sometimes two embryos are transferred.
However, the transfer of two embryos also increases the likelihood of a multiple pregnancy with the associated risk of complications (in particular, the risk of premature birth and low birth weight).
Thus, the probability of a multiple birth is very much increased in the transfer of two embryos from about 2% in the transfer of one embryo to about 28% in the transfer of two embryos, but at the same time the birth rate increases by about 4 percentage points, which can be seen in the following illustration based on data from Germany.
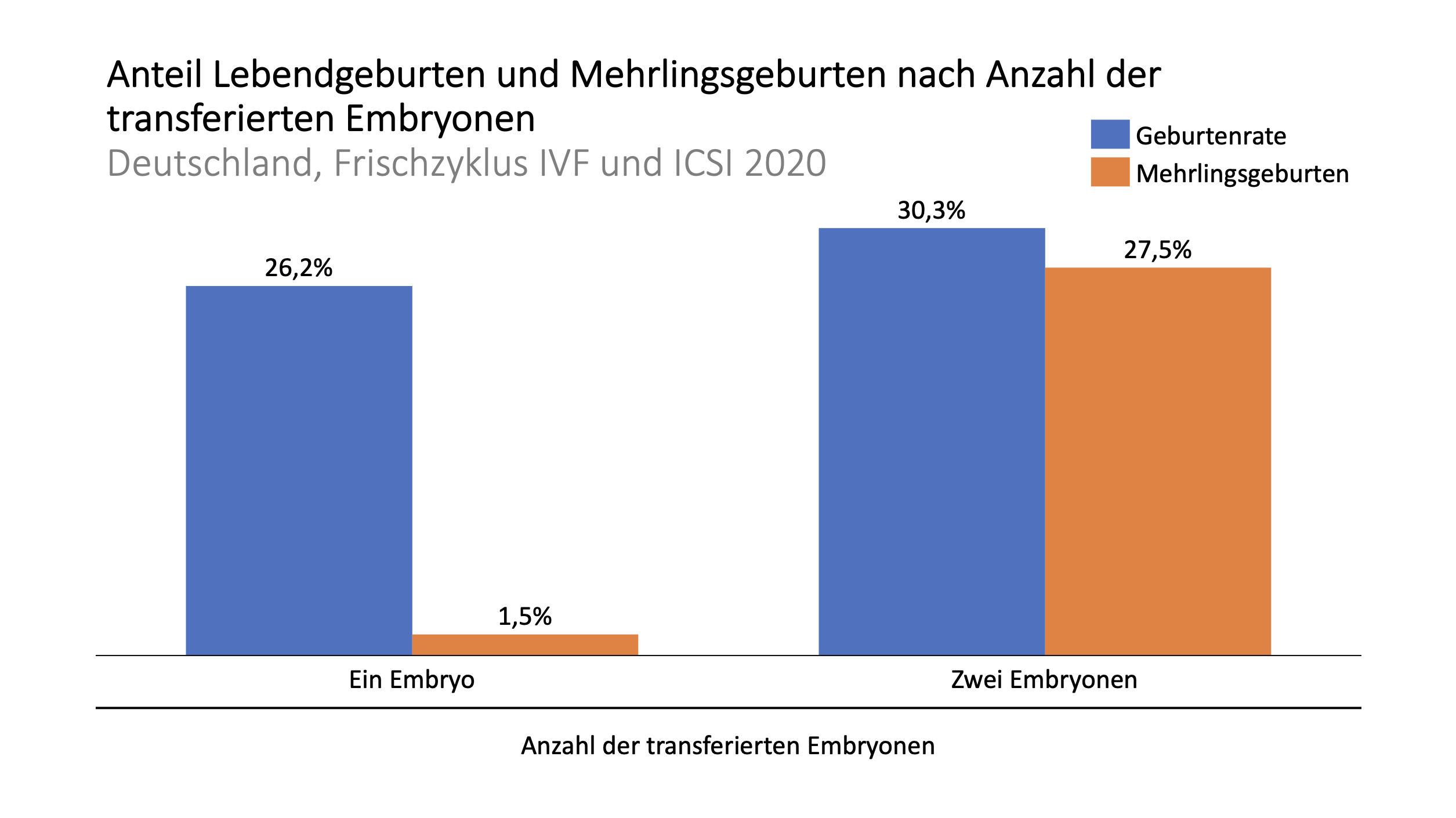
Source: German IVF Register Yearbook 2021
Injuries and inflammations
According to data from Germany, most cases of IVF treatment are without complications, but there are still risks: vaginal bleeding (63% of cases) or bleeding in the abdomen (14%) may occur relatively often during egg retrieval. In addition, peritonitis (~5%) and perineal injuries in women may occur (0.2%).
Rarely, such injuries and inflammations may require hospitalization (1.3% of cases) and/or surgery in the woman (3.5% of cases).
Ovarian hyperstimulation syndrome
Hormonal stimulation of the development of multiple eggs can cause ovarian hyperstimulation syndrome, which causes the ovaries to swell and hurt. In severe cases, this can become life-threatening.
In the past, ovarian hyperstimulation syndrome occurred in up to 10% of women undergoing IVF treatment, nowadays this number is less than 5%, serious cases of ovarian hyperstimulation syndrome occur in less than 1% of women undergoing hormone treatment as part of fertility treatment.
In the case of ovarian hyperstimulation syndrome, it may be necessary, in consultation with the attending physician, to interrupt IVF treatment and temporarily freeze the embryos for later transfer to the woman’s uterus as part of a cryocycle.
How much does IVF cost?
In Switzerland, an IVF cycle usually costs between CHF 4,000 and CHF 9,000, including the hormones used to stimulate egg production. In Germany and Austria, treatment costs are somewhat lower, totaling approximately EUR 3,700 to EUR 5,500 per cycle.
The following table provides an overview of treatment costs in the DACH region and popular destinations for infertility treatment within the European Union – here, significant treatment costs can be saved in particular by IVF treatment in Southern Europe (Greece and Spain) and Eastern Europe (e.g. the Czech Republic).
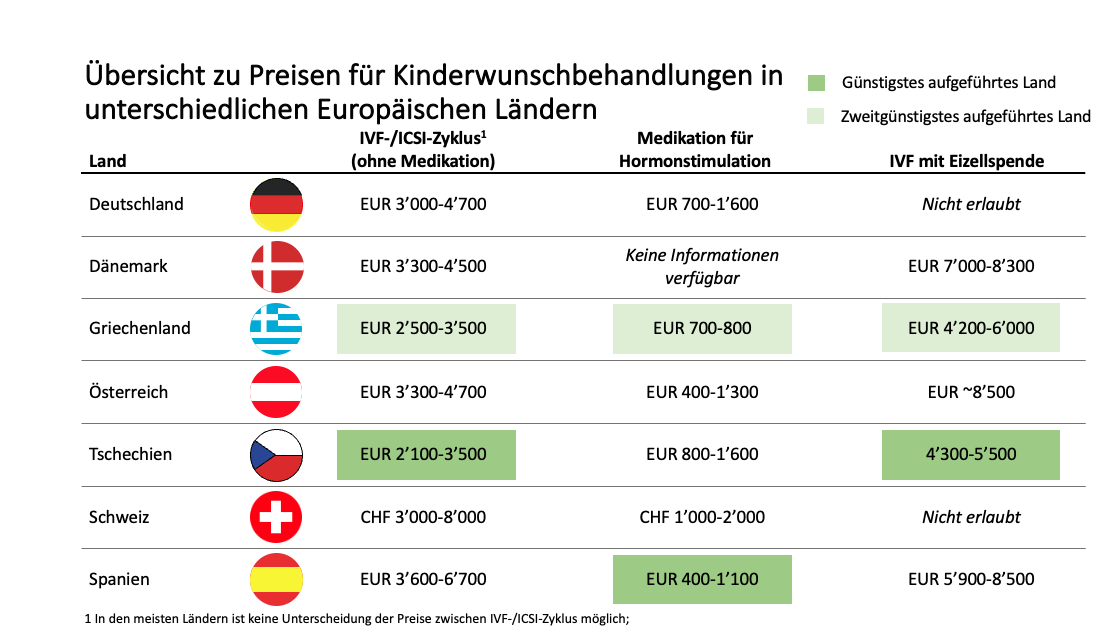
Sources: Fertilityroad.com; various fertility center price lists.
Last update: November 28, 2022
Schwierigkeiten schwanger zu werden, aber die Kosten und Mühen einer Kinderwunsch-Behandlung schrecken Sie ab?
Griechenland gehört zu den europäischen Ländern mit den günstigsten Kinderwunsch-Behandlungen. Bei Kalimedica bringen wir Sie mit Kinderwunsch-Experten zusammen und unterstützen Sie auf Ihrer Reise zur Schwangerschaft



